Are You Suffering from Undiagnosed Low Thyroid?
/Are you suffering from undiagnosed low thyroid?
Have you always suspected you have a sluggish thyroid despite your blood test coming back as “normal”? Well, you are probably right! Most doctors only test the traditional TSH (Thyroid Stimulating Hormone) blood level which, in and of itself, is not a very accurate reflection of thyroid health. It is a measurement of hormone secretion from the pituitary gland, not the actual thyroid levels in your blood. Most integrative physicians know that just ordering a basic TSH test by itself is not good medicine. Dr. Ken Holtorf, M.D. states “the widely held belief that the TSH is an accurate marker of the body’s overall thyroid status is clearly erroneous.”
A more accurate way to diagnose low thyroid is to test for free T3 (triiodothyronine) and free T4 (thyroxine), the actual measurement of thyroid hormone in your blood stream, and not just TSH alone. Dr. Ted Friedman, an endocrinologist at UCLA, recommends to aim for a clinical outcome of FT4 (free T4) and FT3 (free T3) in the upper-normal range, and this way TSH will be suppressed with proper treatment. I personally aim to get the FT3 level above 3.5 pg/ml (Quest Laboratory's reference range for "normal limits" is 2.3 - 4.2 pg/ml).
The other very important (maybe even the most important!) way to assess thyroid function is based upon your symptoms. Laboratory values are often known to be inaccurate so it is important to treat the patient, not the numbers on the lab report. A patient can have supposedly normal thyroid levels but have severe symptoms or, conversely, a patient can have abnormal thyroid labs and exhibit no symptoms. Treat the patient not the labs!
The Classic symptoms of Hypothyroidism
Over 200 symptoms are related to thyroid deficiency but the classic hypothyroid symptoms include:
- Fatigue
- weight gain and puffy face
- depression or lack of motivation
- constipation and/or digestive issues
- dry skin and hair
- cold hands and feet/hypersensitivity to cold
- fibromyalgia/achy joints
- brain fog or poor memory
- heavy or irregular menses
- infertility
- thinning eyebrows
- thinning hair or hair loss
- high cholesterol
Does "Normal" = "Optimal"?
Another problem associated with obtaining only the TSH measurement is its very wide reference range. Essentially this means that the patient can test on the low or high end of the range yet still be considered “normal”. But, as in most testing, there can be a significant difference between optimal and normal! For example, Quest labs lists their reference range for TSH as 0.40 - 4.50 mIU/ml. indicating that a TSH value between 0.4 and 4.5 is considered “normal”. By contrast an optimal level is considered to be between .4 and 1.0 mlU/ml, a significantly narrower tolerance. Put another way, the difference between a person whose TSH value is on the low end of a normal range and a person whose value is on the high end of a normal range can represent as much as 12.13 pounds difference in body weight!
TSH is inversely proportional to thyroid function therefore, the lower your TSH value, the better your thyroid function. Many studies, including the recently published Rotterdam Study (Dec 2016), show that even mild hypothyroidism is a strong indicator of risk for atherosclerosis and heart attack. In fact, there is a two-fold risk for coronary heart disease with even slightly low thyroid function. A low-normal TSH value is good!
So why is your doctor still only testing TSH? Honestly, I don’t know other than to guess they are still practicing what they were taught years ago in medical school and are not aware of the new research on thyroid testing. Conventional doctors usually become alarmed when they see a low TSH. Believe me I’ve had my fair share of disgruntled phone calls from other doctors who assume a low TSH finding indicates Hyperthyroidism (very high thyroid levels) which can cause heart damage and bone loss. But they are confusing a low TSH in a healthy patient, who have optimal levels of free T3/T4, with the low TSH of a hyperthyroid patient suffering from Grave’s disease. Grave’s disease is an autoimmune disorder whereby the body attacks the thyroid gland by producing antibodies that attack TSH receptors. The thyroid gland is stimulated by the immune system causing an overproduction of thyroid hormone levels. The autoantibodies created by the immune system attack not only the thyroid gland but also heart tissue, bones, and eyes. It is apparent therefore that in Grave's Disease patients, as an example, autoantibodies are solely responsible for disease pathology and not, as was previously thought, elevated levels of FT3 and FT4 hormones. An article in the Cortland Forum explains “there are now over 40 studies to show that thyroid replacement does not cause bone loss in healthy patients, even in very high doses."
Are Laboratory values the proper tool for determining treatment guidelines?
So if thyroid lab testing can be unreliable, how do you really know if your thyroid dose is too high? Remember I earlier said that assessing the patient's symptoms was a more important tool for diagnosing thyroid disease than just relying upon lab results. Well, the same rule applies in determining effective dosage of thyroid replacement: if your thyroid dose is too high you will have symptoms of sweating, heart palpitations, racing heart rate, loose bowels and nervousness. If these symptoms arise, there's no need to stop the medication, just lower your dosage or switch to a different formula.
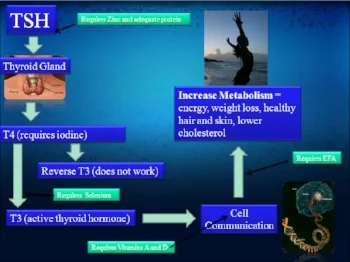
Most doctors just prescribe T4 such as Synthroid, Levoxyl, and Levothyroxine. T4 usually converts into the more active hormone T3. But for a variety of reasons such as aging, stress, illness, dieting, and toxicity, not everyone converts T4 to T3 very well. It is the low T3 (not the TSH or T4) at the cellular level that is responsible for the symptoms of low thyroid. Thus, patients will usually need to be on a combo of both T4 and T3 thyroid hormones. Combo products include Armour Thyroid, West-Throid, and Nature-throid. Patients feel better on both T3 and T4 taken together! There have been several double-blind, randomized, controlled clinical studies showing that patients prefer a combo T4/T3 versus taking T4 alone. For example, The New England Journal of Medicine in 1999 reported findings that patients scored significantly better for mood, energy, concentration, and well-being while on combination therapy as compared to patients receiving T4 therapy alone.
If you are already on thyroid hormone replacement therapy and your labs are normal but you're still experiencing symptoms of low thyroid, you might have “thyroid resistance”. This is similar to Insulin resistance in type 2 diabetics where your cells resist allowing the hormone to permeate the cell membrane to the interior where it is needed. In these cases, patients need a higher dose of thyroid medication (despite normal blood levels!) to drive the hormone across the cell membrane and relieve symptoms. Remember, the goal is to take the dose that makes you feel good again!
So, could you be suffering from Low Thyroid but not know it because you've been tested and your TSH is "normal"? What should you and your doctor consider in making the decision to order lab testing for free T3 and free T4?
Now, suppose you have been diagnosed with Hypothyroidism and placed on thyroid replacement therapy, how will you know if the dosage is too high?
The answer to both questions is the same: pay attention to your symptoms. Get to know what your body is telling you about your hormone levels. You'll know before the labs if your thyroid is too low or too high.
If you would like a good general resource tailored to a patient perspective about thyroid disease diagnosis and treatment please visit www.thyroidchange.org . Aside from interesting articles and blogs, this site offers a wealth of approachable outside references.